Applied Behavior Analysis (ABA) practice owners and managers get incredibly busy. However, just as we expect good Board Certified Behavior Analysts (BCBAs) to consistently graph & monitor data to make program updates for young learners, ABA practice owners need to do the same for their own organizations. In the business context, this is tracking Key Performance Indicators (KPIs) that indicate the health of an ABA practice. When KPIs like cancellation rates or staff attrition start to spike, it can have serious consequences for the business which may not be able to continue operating if updates aren’t made. Selecting appropriate interventions using Organizational Behavior Management (OBM) strategies to get KPIs back on track is important to give time to. Let’s explore how to measure the value of OBM interventions to decide whether they’re worth implementing or not.

What Are OBM Interventions
Simply put, OBM interventions are tactics implemented to target specific behavior for change in an organization. For example, a clinic with employees who are gossiping so much it’s causing coworkers to resign has a problem with gossip behavior. If we believe the function of the group’s behavior to be seeking attention, the Director and others could give non-conditional reinforcement (NCR) in the form of attention when they see the group.
Another OBM intervention could be for the scheduling department. Administrative staff in ABA clinics often feel like their work is secondary to clinic staff, but it’s not. This can show up in employee engagement data. Simple OBM interventions to increase employee engagement for schedulers could be things like graphing the amount of rescheduled sessions and displaying them for others to see in the clinic for increased focus on their work.
Another OBM intervention could be for the scheduling department. Administrative staff in ABA clinics often feel like their work is secondary to clinic staff, but it’s not. This can show up in employee engagement data. Simple OBM interventions to increase employee engagement for schedulers could be things like graphing the amount of rescheduled sessions and displaying them for others to see in the clinic for increased focus on their work.
Measuring Value of OBM Interventions
To measure the value of an OBM intervention, we need to know a few things:
This is quite similar to selecting interventions for young learners. Of course not all interventions are affordable or practical and we need to select the right ones.
Cost Of Doing Nothing
We need to see what current behavior is costing the organization. You may have to combine a few data sources to get to an estimate, but it should be possible. For example, if we want to target last minute client cancellations for reduction, we start with determining how many last minute cancellations there were. Acclaim Autism defines last minute client cancellations as within two hours of the scheduled start time. When this happens, staff are paid for the length of the session up to 3 hours. Using the Electronic Health Record (EHR), we can pull the number of last minute client cancellations, multiply that by the staff’s hourly rate with a little extra for taxes, and come to know how much last minute cancellations cost the organization over a given time period. Let’s call it $20,000 per month for arguments sake. If you want to get fancy with calculations you could add in the cost of replacing the disgruntled Registered Behavior Technicians (RBTs) that resigned over last minute cancellations too. Measure outputs, not behavior. It’s far simpler, and more cost effective.
Process To Pinpoint Behavior for Intervention
Let’s start with defining analyzing the business result or KPI that needs improvement, and work backwards. From the KPI, there should be some kind of permanent product (output) that’s measurable and makes up the KPI. Then, what behavior results in the permanent product, and what are influences on the said behavior. We analyze in this order:
Once we know the behavior and influences on behavior, we can ask: What can we manipulate in the environment that will result in change?
That’s how we come up with possible interventions.
That’s how we come up with possible interventions.
Selecting an OBM Intervention
We then need to propose an intervention and estimate the cost of implementing it. In one organization, the Scheduling team implemented a 3-step warning system to families with a history of last minute cancellations, with messaging getting more serious with more frequent cancellations. Schedulers spent about 2 hours a week managing this system, which is only about $500 a month in time considering all the locations involved.
Determine Possible Savings
Now, what would the savings be to the organization if this OBM intervention was successful? Of course last minute cancellations will never be zero. If last minute client cancellations are reduced by just 10%, that’s $2,000 in savings each month (10% of $20,000 spent on last minute cancellations).
If we estimate 10% savings from this intervention, the value of the intervention is $1,500 per month ($2,000 savings minus $500 cost to implement), or $18,000 per year. That doesn't even account for a likely increase in RBT satisfaction and associated retention.
Putting our Scientist-Practitioner ABA hats on, we know not all interventions are created equal or effective and we’ll need to try different things. We start with what the current behavior costs the organization, hypothesize functions of behavior and interventions that could help, and stack rank them. The most cost-effective or easiest to implement will often be selected.
If we estimate 10% savings from this intervention, the value of the intervention is $1,500 per month ($2,000 savings minus $500 cost to implement), or $18,000 per year. That doesn't even account for a likely increase in RBT satisfaction and associated retention.
Putting our Scientist-Practitioner ABA hats on, we know not all interventions are created equal or effective and we’ll need to try different things. We start with what the current behavior costs the organization, hypothesize functions of behavior and interventions that could help, and stack rank them. The most cost-effective or easiest to implement will often be selected.
OBM Intervention Example: Medical Billing
Here’s a simple dollars and cents example of OBM interventions. In one ABA therapy company, the medical billing wasn’t being managed as effectively as it could be. The KPI is claims $ that are over 90 days old.
Insurance contracts require payment within 30 days for clean claims, so even if there was a denial that was worked correctly, little to no claims should be more than 90 days old. However from February through May 2025, claims over 90 days old grew by approximately $8,590 per week - that could amount to $446,704 per year - an amount too large for most ABA companies to afford to lose if not corrected.
The business results / KPIs were too few claims being paid in less than 90 days. Working backwards, the owner started tracking how many dollars ($) for claims that were submitted to insurance were over 90 days old, investigating the claims history, how claims were resubmitted, how they were submitted in the first place by the billing team, and what was wrong with the claims.
Upon doing an OBM assessment it was clear the billing team was submitting some claims incorrectly without paying much attention to certain details. When those claims were denied, they were resubmitted again or appealed.
Let’s work backwards through four steps to see what the behavior & influencers were:
Insurance contracts require payment within 30 days for clean claims, so even if there was a denial that was worked correctly, little to no claims should be more than 90 days old. However from February through May 2025, claims over 90 days old grew by approximately $8,590 per week - that could amount to $446,704 per year - an amount too large for most ABA companies to afford to lose if not corrected.
The business results / KPIs were too few claims being paid in less than 90 days. Working backwards, the owner started tracking how many dollars ($) for claims that were submitted to insurance were over 90 days old, investigating the claims history, how claims were resubmitted, how they were submitted in the first place by the billing team, and what was wrong with the claims.
Upon doing an OBM assessment it was clear the billing team was submitting some claims incorrectly without paying much attention to certain details. When those claims were denied, they were resubmitted again or appealed.
Let’s work backwards through four steps to see what the behavior & influencers were:
Even following the claims process, appeals were submitted without much customization - just generic appeal language sent to the insurance company’s P.O Box. During the February-May timeframe, it was suggested the team do more to customize the appeals and push insurance companies to approve these claims, while fixing any billing errors based on feedback. However, nothing changed.
A few OBM interventions were considered:
Notice the interventions are ordered from least to most expensive. If we estimate a BCBAs time at $100 per hour to develop an intervention and implement it, we can calculate:
Doing all four interventions makes good sense to see what works; even the cost of all three OBM interventions to save a potential of $447,704 makes sense. The below graph shows the dollar amount of claims outstanding over 90 days old over the time periods in question.
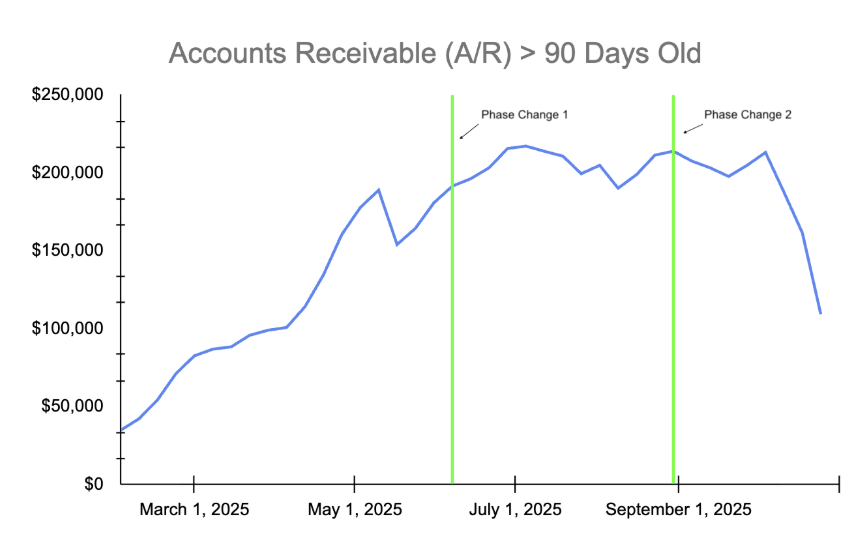
Formal job aids tried and failed in this case. They were implemented within the February-May timeframe, but as you can see in the above graph, the old claims continued to pile up, unpaid.
Although valuable for training future billers, the problem wasn’t a lack of knowledge, it was a motivation deficit that needed to be addressed as opposed to a skill deficit. Data was graphed and shared. It helped demonstrate the problem but didn’t result in any change to motivation (NOTE: a performance management system was introduced for this team recently which should help with motivation).
Phase Change 1 in the graph shows when a medical biller intern was brought on. The intern was highly motivated to do well and bring down the volume of old claims since they wanted a full-time job upon graduation. New claims being submitted had higher approval ratings, stemming the flow of aging claims. However, the existing old claims remained unpaid.
Phase Change 2 in the graph shows when a quality control process was implemented. Every appeal that was submitted to insurance was required to be reviewed by two senior leaders in the organization. They made sure appeals were detailed enough to show the organization submitted claims on time (with proof), followed up regularly, and the claims should have been paid. The individualized appeals helped a great deal. One senior leader worked with the billing team to reach out to insurance companies directly and ask people to review appeals that were submitted. The conversations also helped a great deal.
As you can see in these data, the quality control OBM intervention helped the most to bring down the volume of old claims. Showing the graphed data to the billing team now acts as a form of positive reinforcement for all the great work being done to collect claims in a more timely manner. The $10,600 for this intervention was paid back quite quickly, with the organization collecting over $75,000 in claims over 90 days old within a few months. In business terms, the Return On Investment (ROI) is 601%, calculated below:
Although valuable for training future billers, the problem wasn’t a lack of knowledge, it was a motivation deficit that needed to be addressed as opposed to a skill deficit. Data was graphed and shared. It helped demonstrate the problem but didn’t result in any change to motivation (NOTE: a performance management system was introduced for this team recently which should help with motivation).
Phase Change 1 in the graph shows when a medical biller intern was brought on. The intern was highly motivated to do well and bring down the volume of old claims since they wanted a full-time job upon graduation. New claims being submitted had higher approval ratings, stemming the flow of aging claims. However, the existing old claims remained unpaid.
Phase Change 2 in the graph shows when a quality control process was implemented. Every appeal that was submitted to insurance was required to be reviewed by two senior leaders in the organization. They made sure appeals were detailed enough to show the organization submitted claims on time (with proof), followed up regularly, and the claims should have been paid. The individualized appeals helped a great deal. One senior leader worked with the billing team to reach out to insurance companies directly and ask people to review appeals that were submitted. The conversations also helped a great deal.
As you can see in these data, the quality control OBM intervention helped the most to bring down the volume of old claims. Showing the graphed data to the billing team now acts as a form of positive reinforcement for all the great work being done to collect claims in a more timely manner. The $10,600 for this intervention was paid back quite quickly, with the organization collecting over $75,000 in claims over 90 days old within a few months. In business terms, the Return On Investment (ROI) is 601%, calculated below:
Of course, more should be collected as time goes on, making this intervention even more worthwhile. Behavior has changed, and so have the permanent products (outputs), resulting in better business results.
Selecting and measuring the value of OBM interventions sometimes is easy when claims are involved. In other cases, calculating people’s time and compensation helps determine value based on money spent and saved. Of course there are other considerations too, like impact on client’s progress towards goals which is why we’re all in this field to begin with. Assigning value to things helps us rank and select the most appropriate interventions so we can make better decisions based on data.
ABA practice owners can reach out for support any time. We don’t do paid consulting, and are simply happy to have conversations with like-minded BCBAs trying to improve the field.
Jamie Turner
MBA, PMP, BCBA

